Implantation problems: bone tissue atrophy, bone quality
Machine translation
Original article is written in RU language (link to read it).
Due to the loss of teeth, a decrease in the functional load in the area of the defect in the dental arch on the jaw, over time there are signs of increasing local osteoporosis and atrophy of the alveolar bone occurs. These processes occur most quickly in the bone tissue of the upper jaw.
Long-term studies have shown that during the first three years after tooth extraction, the alveolar process loses about 40-60% of bone matter, then atrophy slows down significantly, bone loses no more than 1% annually.
Read more about the choice of treatment tactics for severe bone tissue atrophy in the online course Inclined implants: immediate rehabilitation for severe bone tissue atrophy .
Destabilization of the occlusion over time causes the loss of remaining teeth; after 65 years, approximately 98% of people are diagnosed with edentia, and 25-40% of patients are diagnosed with complete edentia.

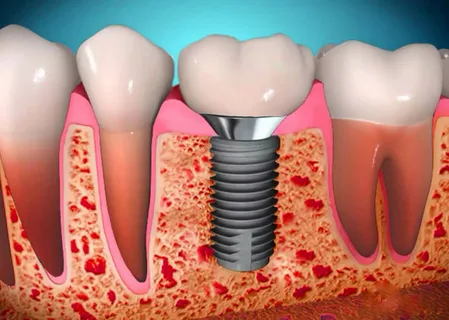
Figure 1. Bone atrophy in the area of extracted teeth.
When planning and performing implantation, the main indicators that the doctor must take into account are the quality and volume of preserved bone tissue:
width of the alveolar bone in the buccolingual dimension,
the volume of bone substance in the interdental spaces, between the remaining teeth,
the thickness of the bone layer above the mandibular canal, as well as in the projection of the bottom of the maxillary sinus,
height of resorption of the alveolar process, jaw body,
thickness of the cortical plate,
ratio of spongy and compact substance.
It is also important to assess the architecture of the alveolar bone. It is customary to distinguish the following types of bone architectonics:
Type I – bone substance is characterized by high density, the space of the spongy layer is filled with powerful trabeculae, the thickness of the layers of compact and spongy substance is in a ratio of 2:1;
Type II - the bone substance is characterized by medium density, the space of the spongy layer is filled with structurally developed trabeculae, it is surrounded by a two- to three-millimeter compact substance, the ratio of the thickness of the compact and spongy substance is 1:1 or 0.5:1;
Type III - bone substance is characterized by low density, thin, few trabeculae are defined in the spongy layer, it is surrounded by 1.0 mm of compact substance, the layers of compact and spongy substance are in a ratio of 0.5: 1.
Today, the most appropriate classification of the degree of bone tissue atrophy is considered to be that proposed by S. Misch and K. Judi, which focuses directly on planning dental implantation. According to their classification, with partial loss of teeth, four groups of bone thickness are distinguished, and with complete loss, another fifth.
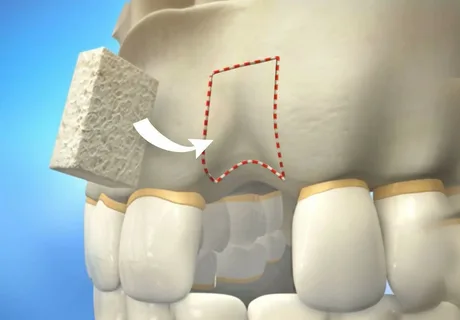
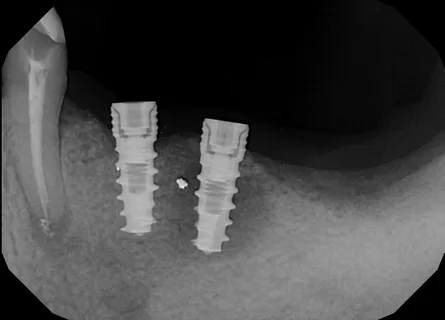
Figure 2. Correction of the area of atrophy.
The classification is based on the assessment of three key characteristics of bone tissue:
width,
height,
mediodistal length.
The authors divide toothless jaws into partially and completely toothless.
Classification for complete edentia according to S. Misch and K. Judi
Group A: the thickness of the bone substance is sufficient to install implants on both jaws, however, in the lower jaw, despite favorable indicators, implants are placed in the space between the mental foramina. Next, fixed prosthetics are shown - these are bridges or removable structures.
Group B: bone substance of a smaller volume is determined. In both jaws, cylindrical or screw implants can be considered, but the size should be smaller. The prognosis for treatment is less favorable and is determined mainly by the quality of bone tissue. The number of support heads increases, which makes it possible to create a large area of the near-contact area along the perimeter of the implant, which will ensure redistribution of the load.
Group C: the preserved thickness of the bone substance in the lower jaw is sufficient for placement of shortened screw and cylindrical implants in the area of the intermental openings. The inferior alveolar nerve may need to be repositioned if the picture is less favorable. If the patient is not embarrassed by the initial situation, intraosseous implants are not installed. A surgical intervention is required to increase the height of the bone crest and raise the bottom of the maxillary sinus.
Group D: the alveolar ridge and basal bone fragments are atrophied. The installation of intraosseous implants is contraindicated. Planning prosthetics using implants after plastic surgery and bone augmentation.

Figure 3. Implantation in the upper jaw.
Classification according to S. Misch and K. Judi for partial edentia involves the identification of 4 classes. Classes are in turn divided into groups.
Classes 1 and 2 of group A: characterized by preservation of teeth in the frontal part of the dental arch. Sufficient thickness of the preserved bone for installation of bridges against the background of included and end defects. Design options: bridges supported by a tooth and implants, or a single implant. The number of implants is determined by the number of teeth removed.
Class 2 group B: the volume of bone substance is slightly reduced, but it is quite sufficient for the installation of screw and cylindrical structures of small sizes. Depending on the clinical situation, it is possible to place several implants. Flat implants are suitable, which are indicated when the volume of bone tissue is reduced.
Class 2 group C: the volume of bone tissue is small, installation of cylindrical and screw structures is impossible. Preliminary surgical preparation is necessary.
Class 2 group D: characterized by deep atrophic processes in the thickness of the bone. Removable designs are recommended. Due to the close location of the mandibular canal, a frequent complication of prosthetics is paresthesia. To prevent a jaw fracture, augmentation of the alveolar part with biomaterials is required.
Classes 3 and 4, group A: characterized by the absence of single or grouped teeth; the bone volume is sufficient to accommodate screw, flat or cylindrical implants. The number of implants is determined by the length of the toothless jaw fragment and the choice of the planned orthopedic design. It is possible to support the prosthesis on implants alone, or on implants and remaining teeth.
Classes 3 and 4, group B: characterized by the presence of extensive toothless fragments, the volume of bone substance is sufficient to accommodate the implants necessary to provide support for fixed orthopedic structures. Preference is often given to flat implants.
Classes 3 and 4, group C: extended areas of bone without teeth, endosseous implants are contraindicated. Preliminary plastic surgery is required to raise the sinus floor and increase the isolation of the inferior alveolar nerve. In a Class 4 clinic, careful use of shortened screw and cylindrical implants may be considered.
Grades 3 and 4, group D: bone atrophy is so significant that endosseous implants are completely excluded. It is recommended to manufacture partial removable structures.

Figure 4. Preliminary sinus lift.
The most suitable type of bone tissue, most suitable for endosseous implantation, according to many experts, is thick porous-compact bone. As teeth are lost and the functional load to which bone tissue is normally exposed decreases, local osteoporosis progresses in the area of the dental arch defect, atrophy of the alveolar ridge occurs, and this process is most noticeable in the lateral areas of the lower jaw.
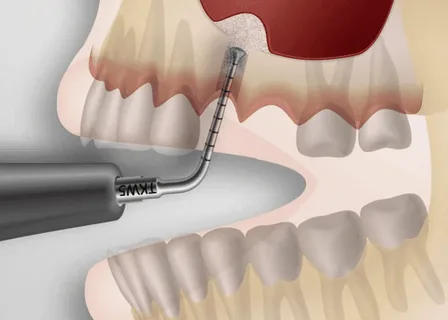
Figure 5. Sinus lift.
A decrease in the mass of bone tissue in the area of the toothless fragment in the upper jaw, which develops due to increasing bone atrophy, makes it difficult to use intraosseous implantation due to the high risk of penetration of the bottom of the maxillary sinus. If the height of the alveolar ridge in the upper jaw is 8-9 mm or less, osteoplastic surgery, “sinus lift,” is recommended, which involves building up bone tissue in the area of the planned implantation by raising the level of the bottom of the maxillary sinus.
If the height of the alveolar ridge in the area of extracted teeth in the lower jaw is 10-12 mm or less, in order to create conditions for implantation, an intervention aimed at shifting the position of the inferior alveolar nerve is recommended.
Despite the long-term effectiveness of such surgical interventions and the skills of the specialists who perform them, some authors believe that treatment tactics must be based on adapting the design to the anatomical nuances of the jaw, and not vice versa.
Updated classic sinus lift protocols on the online course Sinus lift: updated classic and newest proprietary protocols .