Routine ear canal and tympanic membrane inspection after temporomandibular joint arthroscopy
Temporomandibular joint (TMJ) arthroscopy, although considered to be a safe technique by several authors, is not exempted of surgical complications, ranging from 8% to 23%. Due to the proximity of the TMJ, changes in the auditory system after arthroscopy have been reported. Otologic complications range from small lacerations in the external auditory canal to serious tympanic membrane and middle ear injuries. Blood clots and lacerations of the external auditory canal are the most common complains. Lacerations of the ear canal can occur due to anatomical variations and inaccuracies in the introduction of trocars/instruments. The origin of the clots is attributed to blood flowing into the external auditory canal and their adherence to the ear canal and/or tympanic membrane. These can be partially prevented in level 1 and 2 arthroscopies by using a protective gauze in the ear canal, but in a level 3 arthroscopy, when performing transtragal access, the protective gauze needs to be removed and minor bleeding to the ear canal is expected. Most of the time, the surgeon is not aware of these complications intraoperatively, and they are noticed only in the early days after the intervention. In this letter, the authors describe a simple and safe method to observe the ear canal and tympanic membrane after TMJ arthroscopy to detect eventual lesions immediately after the surgery and also to remove inconvenient blood coats from the ear canal.
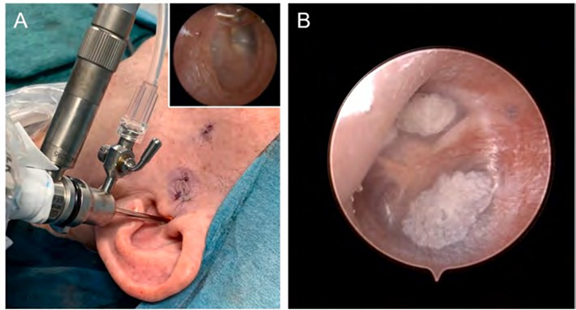
Upon completing the TMJ arthroscopic treatment, we suggest to introduce the arthroscope in the ear canal with the outer protective cannula and the irrigation system (Fig. 1A). A smooth irrigation can be performed to eliminate eventual blood clots. Sometimes, a more continuous irrigation and aspiration is needed to clean the ear canal. After the removal of eventual blood clots, it is recommended to perform a smooth progression with the arthroscope until the tympanic membrane is identified. Proper observation is recommended. The authors also consider it important to register a photography/video, which may be eventually necessary for legal considerations. After this inspection, the arthroscope is slowly removed, and the ear canal is observed to notice eventual lacerations. A 1.9 mm arthroscope with a 30º angle view, including a video system, with a 2.8 mm outer protective cannula (Stryker, San Jose, CA, USA), is used in our practice. The irrigation is gently performed with Ringer’s lactate solution, taking advantage of the connection used during the surgery. The unilateral inspection takes around 1 minute and 30 seconds. The authors recommend attention in this inspection and performing a gentle and smooth entry into the ear canal to avoid any iatrogenic complications of this inspection.
Otologic complications after TMJ arthroscopy are considered a cause of discomfort to the patient and anxiety to the surgeon in postoperative period. The technique presented in this letter is a simple method to check the integrity of the auditory system after the surgery and can contribute to surgeon and patient tranquility. We started to implement this technique routinely after TMJ arthroscopy, and currently, more than 100 ears were verified with this approach. So far, the authors observed no tympanic or ear canal alterations. Sometimes, accidental findings are reported, as demonstrated in Fig. 1B. A 24-year-old female patient underwent bilateral TMJ arthroscopy. During the tympanic membrane inspection, the authors found changes in the membrane and referred the patient to otorhinolaryngology. The diagnosis was myringosclerosis (i.e., calcification of plaques in the tympanic membrane). Apart of those rare and unexpected situations, most of the cases had blood clots, which were easily removed with smooth irrigation. In level 1 TMJ arthroscopy, as the risk of tympanic membrane and ear canal lacerations is very reduced and, sometimes, the TMJ surgeon can have little experience with the arthroscope, the authors do not recommend performing this inspection routinely, with the exception of when intraoperative bleeding is observed, leading to a possible presence of blood clots in the canal. In level 2 and 3 TMJ arthroscopies, we highly recommend performing this inspection.
We reinforce the importance of getting adequate training with arthroscopy, especially for those who do not perform this procedure regularly, since it may lead to unexpected iatrogenic damage to the tympanic membrane and external ear canal.
To summarize, the main advantages of this technique are: (1) early detection of an eventual complication; (2) elimination of inopportune blood clots in the ear canal; and (3) documentation of no lesions (for medical protection). Overall, inspection of the tympanic membrane and ear canal after TMJ arthroscopy is a simple and safe surgical refinement, allowing the early detection of eventual arthroscopic complications.
References:
D.F. Ângelo, R.A.D. Araújo, D. Sanz, Surgical complications related to temporo-mandibular joint arthroscopy: a prospective analysis of 39 single-portal versus 43 double-portal procedures, Int. J. Oral Maxillofac. Surg. 50 (2021) 1089–1094, https://doi.org/10.1016/j.ijom.2020.07.020.
R. González-García, F.J. Rodríguez-Campo, V. Escorial-Hernández, M.F. Muñoz- Guerra, J. Sastre-Pérez, L. Naval-Gías, J.L. Gil-Díez Usandizaga, Complications of temporomandibular joint arthroscopy: a retrospective analytic study of 670 arthroscopic procedures, J. Oral Maxillofac. Surg. 64 (2006) 1587–1591, https://doi.org/10.1016/j.joms.2005.12.058.
M. Tsuyama, T. Kondoh, K. Seto, J. Fukuda, Complications of temporomandibular joint arthroscopy: a retrospective analysis of 301 lysis and lavage procedures performed using the triangulation technique, J. Oral Maxillofac. Surg. 58 (2000) 500–505, https://doi.org/10.1016/s0278-2391(00)90010-7. ; discussion 505-6.
S.K.R. Chowdhury, V. Saxena, K. Rajkumar, R.A. Shadamarshan, Complications of diagnostic TMJ arthroscopy: an institutional study, J Maxillofac Oral Surg 18 (2019) 531–535, https://doi.org/10.1007/s12663-019-01202-3.J. Fernández Sanromán, A. Costas López, M. Fernández Ferro, A.L. de Sánchez, B. Stavaru, J. Arenaz Bua, Complications of temporomandibular joint arthroscopy using two-portal coblation technologies: a prospective study of 475 procedures, J. Cranio-Maxillo-Fac. Surg. 44 (2016) 1221–1225, https://doi.org/10.1016/j.jcms.2016.06.027.
D.F. Ângelo, A. Moreira, D. Sanz, R. São João, Hearing changes after temporo-mandibular joint arthroscopy: a prospective study, Int. J. Oral Maxillofac. Surg. 50 (2021) 1491–1495, https://doi.org/10.1016/j.ijom.2021.02.013.
B. Schickinger, W. Gstoettner, C. Cerny, J. Kornfehl, Variant petrotympanic fissure as possible cause of an otologic complication during TMJ arthroscopy. A case report, Int. J. Oral Maxillofac. Surg. 27 (1998) 17–19, https://doi.org/10.1016/s0901-5027(98)80089-1.

/social-network-service/media/default/6809/fbab08d0.jpg)
